Laser eye surgery is a very popular procedure for correcting near- and far-sightedness as well as astigmatism. Since the first techniques were developed in the early 1980s, many millions of people have gone under the laser hoping to eliminate the need for contacts and glasses. I myself underwent PRK in July, 2011. As is my nature, before I leapt, I looked very closely at the available information on laser eye surgery. What I found was surprising, even disturbing.
If you think there is only one type (or ten types) of laser eye surgery commonly performed, you are seriously under-informed about the entire procedure.
It wasn’t until I spent a great many hours investigating the procedure in detail, that I realized how stunningly little information is available to those who are performing their own casual investigation into laser eye surgery. I am dismayed at the lack of information or the outright misinformation provided by practitioners of the surgeries, no doubt in order to prevent scaring off their potential clientele.
The truth is that there are a huge variety of laser eye surgeries, all masquerading under one or two common names. If you think there is only one type (or ten types) of laser eye surgery commonly performed, you are seriously under-informed about the entire procedure. For example, two people, each having had the Lasik variety of surgery performed, could have had completely different surgeries, using completely different procedures, and with completely different risks, side-effects, and expected outcomes.
It is absolutely critical to know exactly why you would choose PRK, Lasek, Epi-Lasik, or especially Lasik.
I hope the following article will provide prospective patients a strong base-level of necessary understanding of the currently available methods of laser eye surgery. Rather than trusting what I provide here as gospel, I prefer that the reader take this article as a jumping-off point for their own education.
For reasons that will become readily apparent after reading this article, I strongly recommend against the corneal flap-based Lasik procedures. Ultimately though, you must find your own answers. Before undergoing surgery, you should educate yourself on the risks involved, you should know what questions to ask of a potential surgeon, and most importantly, it is absolutely critical to know exactly why you would choose PRK, Lasek, Epi-Lasik, or especially Lasik.
While I will discuss some important areas of risk, especially the risk differences between the various procedures, this won’t be an exhaustive risk analysis of laser eye surgery. Each prospective patient should find their own answers to these questions through self-guided research and through conversations with their (hopefully independent) ophthalmologist and their potential eye surgeons. It is my hope however that, after reading this article, those looking into the surgery will have a better idea of just what questions they will need to find answers to.
Contents
A Brief Look at Eye Anatomy
Before we begin with the details of laser eye surgery, we need to establish the relevant structure of the eye, specifically the cornea, the transparent part of the eye which covers the iris, pupil, and interior parts of the eye.
The cornea is comprised primarily of the Stroma, with a layer of transparent skin, the Epithelium, covering it. The average corneal thickness in a Caucasian is about 540 µm (about 0.5 mm); it is less in Blacks (520 µm) and even less in Asians (490-510 µm). These are average values, and each individual’s corneal thickness can vary by a significant amount. As I’ll discuss further down, these variances can have very large effects on the risks of the various laser procedures.
The cornea’s structural integrity is always compromised; how much depends greatly on which type of laser surgery is chosen.
In addition to performing about two-thirds of the focusing power of the eye (with the adaptive lens performing the remainder), a very important role of the cornea is to provide structural integrity of the eye. When intraocular pressure is too great, or the cornea is otherwise unable to resist against the pressures within the eye, serious conditions such as ectasia or keratoconus (bulging of the cornea, requiring transplant) can result.
Because all methods of laser eye surgery involve some level of cutting or reshaping of the cornea, the cornea’s structural integrity is always compromised; how much depends greatly on which type of laser surgery is chosen. The difference of just how much cornea is cut between the different methods may surprise you, and should be the paramount consideration when choosing a laser eye surgery method.
The Many Flavours of Laser Eye Surgery
The first step in understanding laser eye surgery is to examine the various procedures that fall under the broad umbrella of the term. The variations between different surgeries can be grouped as follows:
- Where the correction is made and how the site is accessed.
- Mid-Cornea – Cornea Flap: Lasik
- Cornea-Surface
- No Flap: PRK
- Skin-Only Flap: Lasek and Epi-Lasik
- How the correction ‘prescription’ or ‘map’ is developed.
- General Prescription Map
- Semi-Custom Preset Map
- Fully Custom Map
- How the eye is tracked and the laser is aimed.
- Outside vs Inside Iris Tracking
- 3D vs 2D Tracking
- Tracking Speed
- Outside vs Inside Iris Tracking
- How the correction is applied to the eye and the size of treatment zone.
- Correction Zone Only vs Correction Zone with Tapered Edge
- Correction/Tapered Zone Larger/Smaller than Dilated Pupil
- Correction Zone Only vs Correction Zone with Tapered Edge
As you can see, each of the major category groups contains a number of choices (and sub-choices) which can drastically affect the surgery performed. This makes for a dizzying variety of possible procedures falling under the Laser Eye Surgery umbrella. While some discussions on laser eye surgery focus on comparing Lasik, Lasek, PRK, etc, even this level of detail covers only a subset of the important differentiators, and decision points, that make up just the first grouping above. In order to truly understand the procedure, prospective patients need to look at each of these areas in detail.
In this article, I will focus on just the first major question: where the correction is made. This is the major differentiator between Lasik, PRK, Lasek, etc. For more information about the subsequent (important!) questions, see my article: My Laser Eye Surgery, Part I: PRK Pre-Op Preparation.
Critical Decision: Correction Site and Access: Lasik vs PRK
The most critical decision in choosing a laser eye surgery procedure is selecting where the correction is made and how that correction site is accessed. The four primary types of laser eye surgery, PRK, Lasik, Lasek, and Epi-Lasik fall within two main categories of where the correction is made: mid-cornea corrections (Lasik) and cornea-surface corrections (PRK, Lasek, and Epi-Lasik). Each procedure (and their sub-types) are refinements on how that correction site is accessed.
Lasik mid-cornea procedures are always more invasive, significantly compromising the biomechanical integrity of the eye.
While each of the differences between the various procedures warrants careful consideration, this factor alone, where the correction is made, has by far the greatest impact on overall short-term and long-term risk of the surgery.
Mid-Cornea Correction: Lasik
The Lasik family of eye surgeries, including the various ‘all laser lasik’ procedures (but not epi-lasik, see below) all involve cutting a flap into the cornea (some with a blade, others with a laser), folding that flap back, performing the correction mid-cornea by burning or more accurately vaporizing a lens shape in your cornea, and then finally re-seating the corneal flap. These mid-cornea procedures are relatively new compared to the much older cornea-surface procedures.
As illustrated above, the flap-based correction method involves cutting a significant way through the structure of the cornea, before any corrective shaping is performed. As a result of this, Lasik mid-cornea procedures are always more invasive, significantly compromising the biomechanical integrity of the eye.
This graphic illustrates an average 150µm cornea-flap cut (see the section below on the variability of Lasik cornea flaps), with 1-10 diopter mid-cornea corrections. Note that, since the creation of this graphic, among some practitioners, the 250µm ‘safe’ residual thickness is being revised to 300-350µm.
Cornea-Surface Correction: PRK, Lasek, & Epi-Lasik
The cornea surface procedures, PRK, Lasek, and Epi-Lasik, all involve removing only the epithelium, the skin layer which covers the cornea, and then performing the correction by reshaping the surface of the cornea. With PRK (pictured below), the skin layer is loosened by an alcohol bath, removed completely via a blade, and then allowed to grow back over the cornea after surgery. With Lasek and Epi-Lasik, the skin layer is loosened by an alcohol bath (all Lasek and some Epi-Lasik), a skin-only flap is created via a blade, and then re-seated overtop the cornea after surgery.
As illustrated above, the cornea-surface correction method involves lifting off the epithelium, the skin layer, then correcting the surface of the cornea. As a result, the cornea-surface procedures are the least invasive, retaining the highest degree of biomechanical integrity of the eye.
Each of the surface-ablation methods are quite similar, with the only differences being how the skin is removed and whether or not it is reseated after surgery. Check out the Pros and Cons section below for a more detailed breakdown of each.
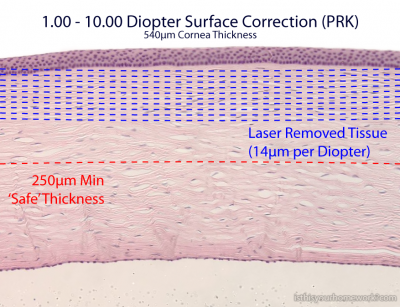
This graphic illustrates 1-10 diopter cornea-surface corrections. Note that, since the creation of this graphic, among some practitioners, the 250µm ‘safe’ residual thickness is being revised to 300-350µm.
Serious Concerns with Lasik
If you haven’t already realized the serious concerns with Lasik, concerns arising over the significant difference between Lasik vs PRK (and the other cornea-surface procedures), I urge you to think intuitively about the procedures.
The ugly truth about Lasik is that the cornea flap never actually heals.
The cut is permanent. The cornea is forever compromised.
Use your instincts when assessing the wisdom of severing a significant portion of the cornea. Ask yourself what purpose the cornea serves (See: ‘A Brief Look at Eye Anatomy’ above) and what potential consequences can arise from compromising it so significantly. Bear those thoughts in mind as you read the following areas of concern with the Lasik procedure.
According to Amoils(1) , LASIK has certain intrinsic problems, and the combination of incisional surgery and laser ablation has a potential for serious short- and long-term problems.
1. The Lasik Cornea Flap Never Heals
First, and most importantly, the ugly truth about Lasik is that the cornea flap never actually heals. The cut is permanent. The cornea is forever compromised. You may hear Lasik surgeons repeating a familiar talking-point that: “Within two years, the lasik flap will be strong enough that any force significant enough to dislodge it, would injure an untreated eye.” This is a lie. It’s a lie told over and over again by countless lasik doctors. They sleep at night by telling themselves that the wound does ‘heal’ in that the skin heals and it creates a bond, however the cornea itself never actually heals, never rebinds together, the flap is permanent.
There’s a catch – that flap never heals after it is gently repositioned. Because there is no scarring the LASIK surgeon can retreat the eye if more laser is needed. Lots of accidental injuries can also lift that flap: shrubbery, children’s fingers, spray from water skiing, eye-pokes from sports competition, etc. LASIK flap trauma can cause the flap to completely come off the eye…bad news!
The cornea flap never heals, only the skin layer overtop of it. There are numerous reports of quite mild trauma, even actions as light as finger rubbing, that have dislodged the flap even up to 14 years after surgery.
There are numerous case reports and small case series of late-onset flap dislocations. Holt et al. recently reported the longest documented interval from LASIK surgery to traumatic flap dislocation at 14 years after LASIK.
In a brief literature search, we found 11 cases that presented at least 24 months after LASIK. We found the majority of dislocations were caused by minor shearing force trauma such as a fingernail injury.
As you’ll see in the following section, the potential consequences of that permanently thinned cornea are incredibly serious.
2. Higher Risk of Permanent Vision Loss Due to Ectasia with Lasik
Ectasia is a stretching and bulging of the cornea, resulting in rapid vision loss, often requiring corneal transplant to treat. The causes of ectasia are manifold, but a significant rise in post-Lasik ectasia has been seen.
The Lasik community has taken the issue very, very seriously. The most frequent topic being discussed by Lasik surgeons in journals and at conferences is the development of methods of pre-screening patients to reduce the rate of post-lasik ectasia.
The true incidence of post-LASIK corneal ectasia is currently unknown. While only 180 cases of post-LASIK corneal ectasia have been described in the published literature – many of which are unexplained – experts believe that anything from 5,000 to 112,000 cases have gone unreported.
The true rate of post-Lasik ectasia may never be known, but estimates have peaked at the 0.6-0.9% rate and with newer screening techniques in place, the current rate is estimated to be about 1 in 2,500.
Yesterday’s wisdom was that 250µm was a ‘safe’ residual thickness, but today’s best practices suggest 300-350µm. What will tomorrow’s ‘safe’ be?
With millions of lasik surgeries being performed, even a 1 in 2,500 chance of debilitating vision loss is far too high for my taste. And that’s only if Lasik doctors turn away as many patients as possible. The risk factors leading to ectasia are still being studied, but the residual thickness of the cornea, coupled with the amount of correction are universally cited as the prime factors. The rates of ectasia are significantly reduced after PRK and other cornea-surface procedures, where less of the cornea is compromised.
Research by John Marshall PhD and others, leading to improved understanding about the lamellar organisation of the corneal collagen fibrils, its relationship with corneal tensile strength and biomechanics, and how the latter is affected by LASIK flap creation and laser ablation, has been the foundation for understanding why the risk of ectasia is lower after PRK versus LASIK as well as for the development of new LASIK techniques, eg, thin-flap LASIK and creation of flaps with an inverted side cut using the femtosecond laser, aiming to better preserve corneal biomechanical stability.
However, while iatrogenic ectasia appears to be far more common after LASIK than after PRK, the exact incidence of post-PRK ectasia is unknown, noted Dr Güell.
Again, the fundamental problem with Lasik rears its head, the cornea is critically important for maintaining the structural integrity of the eye, yet as the two graphics above illustrate, significantly more cornea is compromised by Lasik than by the cornea-surface procedures such as PRK. Yesterday’s wisdom was that 250µm was a ‘safe’ residual thickness, but today’s best practices suggest 300-350µm. What will tomorrow’s ‘safe’ be? Obviously the Lasik industry is coming around to what should be intuitive to everybody, that the more of the cornea that is compromised (both by the flap cut and by the correction itself), the less it is capable to maintain the proper shape of the eye.
Lasik doctors will tell you that incident rates of ectasia are low, but they don’t tell you that they are many, many times higher with Lasik than with PRK.
A survey of the incidence of ectasia following corneal refractive procedures showed that LASIK accounted for 96 per cent of cases while PRK accounted for only four per cent (Randleman et al. Ophthalmology 2008, 115: 37-50).
Prospective patients of any medical procedure understand that there are risks. They understand that there is a trade-off between the potential upside of the outcome versus the potential pitfalls of side-effects. However, many prospective Lasik patients aren’t ever aware that there are alternatives that provide those same upsides, without the serious pitfalls. Lasik doctors will tell you that incident rates of ectasia are low, but they don’t tell you that they are many, many times higher with Lasik than with PRK.
I strongly recommend that anybody considering Lasik, do some serious digging into the phenomenon of post-lasik ectasia. It’s an incredibly serious condition that simple common sense (as well as serious scientific study) reveals is more likely to occur with mid-cornea Lasik procedures, than with cornea-surface PRK procedures.
3. The High Variability of Lasik Flap Thickness
With Lasik, before the correction is even applied, a significant amount of the cornea is sliced into. This is done either via a kind scalpel called a “microkeratome”, or via a specialized laser used only to make the flap, an “IntraLase” laser. However, the thickness of this flap is never consistent from patient to patient, indeed it can vary greatly depending upon both the skill of the surgeon and upon which Lasik variant, microkeratome or IntraLase is chosen (with the latter being somewhat more precise).
Even if you are a ‘good candidate for lasik’, the high variability of the flap thickness could leave you with a much too thin cornea.
Even with the best surgeon using the latest flap-cutting technique, there is still quite a bit of chance involved in just how much of the patient’s cornea is going to be cut into to make the flap. For a somewhat frightening exhibit of this, refer to the abstract from the paper below, which describes differences in the ‘reproducibility’ of Lasik flap thickness between mechanical blade and IntraLase laser flap-cutting methods.
For 99 flaps created using the IntraLase FS laser with an intended thickness of 110 μm, the mean achieved thickness was 119±12 μm (range: 82 to 149 μm).
In 100 eyes treated with the Moria LSK-1 micro-keratome with an intended flap thick-ness of 160 μm, the mean achieved thickness was 130±19 μm (range: 71 to 186 μm).
In 135 eyes treated with the Moria M2 microkeratome with an intended flap thickness of 130 μm, mean thickness was 142±24 μm (range: 84 to 203 μm).
When aiming to cut only 130μm into the cornea, sometimes cutting over 70µm too deep is an absolutely staggering error.
What frightens me about that report is that, while IntraLase flaps are off by more than I’m comfortable with, the flaps cut by surgeons using mechanical blades were sometimes off by huge amounts from what was being aimed for; both types of blade had a range of actual cut thicknesses wider than 115µm. Even if you are a ‘good candidate for lasik’, the high variability of the flap thickness could leave you with a much too thin cornea. When aiming to cut only 130μm into the cornea, sometimes cutting over 70µm too deep is an absolutely staggering error. Indeed using one type of mechanical blade, the incidence rate of “thick flaps”, flaps greater than 170μm, which means cutting significantly deeper into the cornea than intended, was over 10%. Scary stuff.
Most Lasik surgeons have no idea how much corneal thickness their patients have left after surgery.
Indeed, due to the unpredictable flap thickness, the Lasik journals recommend surgeons measure the thickness of the patient’s cornea flap mid-surgery (a procedure called pachymetry), aborting the procedure if the flap thickness will result in a too-thin cornea. Makes sense right?
Well most Lasik surgeons don’t do this.
To preserve enough residual stromal bed, Dr. Trattler added, “it’s most important to measure the patient’s flaps at the time of surgery.” Yet unpublished data from 2005 survey conducted by Magill Research Center at the Medical University of South Carolina found only 34 percent of U.S. refractive surgeons routinely perform intraoperative pachymetry, he said.
Dr. Rabinowitz agreed that pachymetry during surgery is essential because keratomes produce such variation in the thickness of the flap. “You cut the flap and lift it up, then you measure it,” he said. If the measurement is too low, abort the procedure, he said. “If you don’t have enough tissue, a few months later you can do PRK.”
That to me is frightening. There is a huge random variation in flap-thickness, but most doctors don’t even measure the flap. This means most Lasik surgeons have no idea how much corneal thickness their patients have left after surgery.
4. Retreatment is Far More Complicated After Lasik
Because a significant part of the cornea is compromised when cutting the lasik flap, there is obviously significantly less cornea thickness after Lasik. Additionally, because of the high variability of that flap thickness, it is difficult to determine in advance how much flap thickness will remain. This means that, not only is the structural integrity of the eye lessened, and unpredictably so, but the options for retreatment are also severely limited. There is only so much cornea that can be safely burned away, and since Lasik already starts much deeper into the cornea than the cornea-surface options, immediate retreatment to correct errors in the procedure or future retreatment to re-correct changing vision are far more risky, sometimes not even possible.
Even a single Lasik treatment is simply not an option for people with thinner than average corneas or significant vision prescriptions. For these people, the much less risky cornea-surface treatments (PRK, Lasek, epi-Lasik, etc) are still a safe and recommended option. For those with thin, but supposedly ‘safe enough’ corneal thicknesses, they’re rolling the dice as to whether their post treatment eye will still be ‘safe enough’ for retreatment or whether they might be stuck with uncorrectable vision forever.
Not only that, but there can be serious issues with epithelial ingrowth under the flap when a retreatment is attempted. Epithelial ingrowth after Lasik is not exactly unheard of without retreatment, but it is significantly more likely when performing a Lasik retreatment.
Lifting a flap is associated with a higher incidence of epithelial ingrowth than primary procedures. That is why many doctors are going to PRK enhancement on Lasik flaps. Epithelial ingrowth is no fun. The rate of ingrowth in the literature on enhancements ranges from 10% to 40% versus only 1-2% for primary procedures.
Of course, nobody wants a retreatment to correct the first procedure, but it can be necessary. “The re- treatment rate after primary LASIK varies in different studies and is approximately 6% to 20%.” And, because you’re working with a much more compromised cornea after Lasik, the options for retreatment are significantly more complicated.
5. Severe Eye Dryness is Far More Common with Lasik
Many people who have never had laser surgery have dry eyes. It is annoying, sometimes painful. Few of them have found eye dryness severe enough to undergo a surgical procedure to implant plugs to help hydrate their eyes. This is the “dry eye” that is meant in laser eye surgery journals. It is not trivial.
A staggering 1.3% of Lasik patients had to have plugs surgically embedded in their eyes to help offset severe and painful eye dryness.
Immediately after my surgery, I got a feel for this sort of severe dry eye. It lasted a few days while my epithelial layer re-grew after PRK. It was not something I would have wanted to live with for the rest of my life. Unfortunately, many Lasik patients have to endure this, or have additional surgical procedures to help mitigate it.
Another flap-related complication in the study was dry eye syndrome, which in 1.3 per cent of LASIK-treated eyes was severe enough to require implantation of punctal plugs. In contrast, punctal plugs were not necessary in any eyes in the surface ablation groups. [Mr.Temple: "surface ablation groups" means PRK, Lasek, Epi-Lasik]
The greater severing of and slower re-growth of corneal nerves after LASIK, which several studies have demonstrated, is the most likely cause of the procedure’s higher incidence of dry eye, he noted.
Lasik cuts much deeper into the cornea. It severs a lot more nerves than PRK/Lasek/Epi-Lasik. And of course, the deeper you cut (which is unpredictable due to randomness of corneal flap cuts), the greater chance you have of cutting so many nerves that your eyes no longer produce enough tears. A staggering 1.3% of Lasik patients had to have plugs surgically embedded in their eyes to help offset severe and painful eye dryness.
No PRK patients had to have this done. PRK leaves a more intact, more healthy cornea.
If Lasik is so dangerous, why is it so popular?
This is a question worth asking. If Lasik has higher rates of very serious short- and long-term side-effects, why is it so popular.
Lasik is the very definition of a ‘quick-fix’.
Lasik is an easier sell. Lasik patients feel ‘good as new’ just a day or two after surgery. With little discomfort in recovery, Lasik patients tell other prospective patients how easy it was. How great they see the next day. These patients have no idea how much riskier their procedure is over PRK/Lasek/Epi-Lasik, they just know they’re fine now. Lasik is the very definition of a ‘quick-fix’, often it appears easier, but serious problems can occur in the long run.
With PRK, the skin layer of the cornea is removed. Like removing any top-layer of skin, that area is going to be raw until it regrows. PRK has a five-day recovery while your cornea regrows a fresh, seam-free layer of skin under a protective bandage contact lens. These five days are uncomfortable, and painful without medication. Additionally, the skin that grows back is a little swollen for a week or two, this causes slight vision artifacts (ghosting, faint double-images) until the new skin over the cornea completely heals. I describe the preparation and healing process in detail in my series documenting my experience My Laser Eye Surgery, Part I: PRK Pre-Op Preparation.
Now however, there is little difference in recovery between the corneal-compromising Lasik and the corneal-conserving Lasek/Epi-Lasik.
With the newer Lasek and Epi-Lasik procedures the recovery time and experience matches that of Lasik. In these procedures the epithelial skin layer is not completely removed. Instead the skin layer is folded back in a flap (similar to Lasik, but it’s a skin-only flap, not a corneal flap), and then after the correction is made to the cornea, the skin flap is laid back. This is less traumatic to the cornea’s skin, but has its own minor complications with that flap. These complications are significantly less serious than corneal-flap complications. Often, the worst that happens is the Lasek skin-flap simply has to be removed, effectively turning the procedure into a PRK procedure.
I chose to stick with PRK over Lasek/Epi-Lasik (but never Lasik!) mostly because it was the oldest and most studied procedure and the surgeons were more experienced with it. If I was looking at the procedure today instead of in 2011, I may well have chosen an epithelial-flap procedure like Lasek. I would never contemplate the Lasik corneal-flap procedure.
So, in the past there was a significant difference in recovery between Lasik with its corneal-flap, and the safer PRK, with its epithelial regrowth. Now however, there is little difference in recovery between the corneal-compromising Lasik and the corneal-conserving Lasek/Epi-Lasik.
Of course, doctors are still performing Lasik, when in my opinion there is absolutely zero benefit (even over the short term) to the patient compared the alternatives.
So why is Lasik still performed?
Well, it costs money to upgrade a practice from Lasik. New machines, new training, new techniques. What’s the business incentive for a doctor to do this? There is little. Until Lasik is removed as a medically authorized procedure, doctors can tell themselves that incidents of complication are low (which is true, but many times higher than other, equally effective procedures), and continue earning huge amounts of money offering the Lasik quick-fix.
And Lasik is a powerful ‘brand’. When people think laser eye surgery, they think Lasik. Indeed some PRK and Lasek providers are advertising their clinics as Lasik clinics, capitalizing on the brand recognition, while recommending the safer procedures.
What is a prospective patient to do?
The vast majority of prospective patients will never research laser eye surgery. Will never even be aware of the issues described above. That to me is frightening.
I hope the information I’ve provided helps the people who have found this page. Prospective patients should take this information and go do their own research. They should ask their local Lasik/PRK clinics questions about these complications. They should take those answers and try their best to find out how true they are.
Ultimately prospective patients are going to have to make a decision for themselves. Hopefully I’ve helped to make it a well-informed decision.
Good luck, and keep me posted on your journey!
Continued Reading
Here are my posts on PRK and laser eye surgery, continue reading or, feel free to join the discussion in the comments below!
Laser Eye Surgery Primer: Lasik vs PRK
Lasik vs PRK: What the Lasik Doctor Doesn’t Tell You (You are Here)
My Laser Eye Surgery, Part I: PRK Pre-Op Preparation
My Laser Eye Surgery, Part II: The PRK Operation
My Laser Eye Surgery, Part III: PRK Post-Op Recovery
Halos: A Likely Complication of PRK or Lasik
More Information








Dear Mr. Temple,
Thank you for this article. It radically changed the way I’ve perceived LASIK.
-Sasha
Thank you a clear and informative write up.
You explained it clearly. The risks are not worth it. There is another method, the most advanced in the world. It’s called NO TOUCH or TransPRK. It’s used all over the world but here. FDA and AMA are bought off, as usual. It’s short, one minute or less eye surgery, nothing touches your eye. FAST. DONE. One pass, not two lasers. I’m a researcher, paid to research. This German Amaris 750RS or 1050RS is the most advanced in the world, but the USA won’t approve it because an entire industry has evolved to treat bad outcomes. It’s all about the money. Caveat Emptor, Buyer Beware! Go to London or Copenhagen, get NO TOUCH. Be safe. Science has proven fast laser one pass no touch means less loss cornea and faster healing after pain for the usual two weeks. This is what I would do if I had bad eyes.
Thanks for your post. I started researching about TransPRK. It still wasnt very clear to me. So they don’t remove the whole epithelial but only parts of it? (where the cornea needs to be changed)
Can you tell me where in Brazil I could have this thing done? I would prefer Sao Paulo if possible.
Thank you
That’s a tough one. You have to Internet search it to find out.
I know it all started with the London Eye Center using the Amaris 750s and 1500rs I believe it is, most advanced in the world. It’s not available in the USA at all. What some call “no touch PRK” is not, still use chemicals to remove the top layer. The problem is USA and many other countries are far behind the rest of the world in this technology.
I like the Amaris machine because it is fast, like 30 secondsan eye and all done. When the laser doesn’t hurt much if done quickly and less problems.
I have the same problem, I have to go to Denmark or England or maybe Toronto to get it done, not the USA.
I just had “Amaris Less Pain Lasek” in Gangnam, South Korea, last Monday. 1600 cheon-won (roughly dollars) and a lifetime guarantee. At the moment I am quite nearsighted, having been deliberately overcorrected due to anticipated regression. Seeing your information is reassuring that I chose the right procedure. And FYI for everyone here, you can get it in Seoul and they do cater to medical tourism.
Let me know how you made out Barbara? They now have one location more near me in Toronto. I’m in RI. The FDA still has their old favorites in the USA to keep out the Amaris machines, particularly the 1050S and 750S.
Sorry to take so long replying.
The overcorrection was very slightly overcorrected even after 10 months, so I opted to take them up on their lifetime guarantee. I now need 1.25 reading glasses for small print or extended reading sessions, and do not require any glasses for basically anything else. Between surgeries I could read well but needed glasses to see far distance ie ride a bike or drive a car…or see the horizon. The nature nut inside me would not abide.
My eyes are a touch drier than they were before the surgeries but they’ve always run a bit on the dry side. I keep drops handy but only need them under particular circumstances such as running the fireplace last night.
I turned fifty last year, so I’m on par with normal-sighted peers.
Hi Bob,
What is the maximum myopia power can be corrected with the Amaris 750s and 1500rs smart pulse technology.
Doctor who has performed more than 50000 surgeries of all kinds(PRK,LASIK etc.) advised me not to go for PRK as correcting power more than -5 causes haze complication.
Does correction of high power causes haze complication?
My power is -6.25 -0.5 cyl and -6.5.
This study found no significant difference between complications after TransPRK vs alcohol-assisted PRK. No significant difference in pain index either. tPRK even had more instances of corneal haze, although it wasn’t enough to be considered statistically significant. They say this is because tPRK has to fire the laser longer, which increases the temperature of the stroma, which increases risk of haze formation. After tPRK the epithelium does heal more quickly, but that doesn’t mean traditional-PRK does any more permanent damage to the eye.
And as for surgery length, from what I’ve seen tPRK is only about a minute faster than PRK. One minute shorter doesn’t really make any difference to me.
Trying to do my research. Do you have studies you can point me to that say something different?
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4753858/
OK, I’ve seen more, and the lasers you’re discussing are definitely faster than USA models. But still, length of the procedure isn’t much of a selling point for me.
Thank you so much Mr. Temple for your very detailed, informative and funny blog describing your LVC journey. I went for my consultation last week and was undecided which treatment to go with. After reading your blog I am excited to go ahead with the PRK. Thanks as well for the little tips along the way (I’m heading to Costco to get tinfoil to “operation grow-op” my bedroom windows prior to procedure). I’m having my procedure done in Vancouver, BC as well. Wish me luck!! Lolly
How did it go, Lolly?
My son, Max Cronin, age 27 years old, committed suicide 1-15-16, as a direct result of complications he experienced from Lasik. He left suicide letters stating this and kept details of his complications. He experienced vision loss, constant eye pain, dry eyes, haze, and loss of quality of life resulting in depression and his suicide. He was unable to work or continue his life goals due to his eye complications.
As a medical physician, I can definitely state that Lasik complications can lead to suicide.
For an elecive procedure, the risks and long term complications are understated.
The resultant complications and negative quality of life issues increase the risks of depression, attemtpted suicide, and suicide.
Nancy L. Burleson MD
I’m very sorry for your loss, Nancy.
It’s frustrating for me to see that willful understatement and underreporting of complications. I can’t even imagine how it would feel if somebody I loved were affected, especially driven to end their life to escape them.
Thank you for sharing your story, for helping to lead others to make an informed decision.
My mum commited suicide in March last year. She had terrible dry eye, the worst kind. She had Lasik a few years prior. She had special sealed glasses, constant drops in her eyes (special serum) and suffered greatly. I somehow didn’t connect the two before seeing this, thinking it was a smaller part amongst other issues. Enlightening thank you
Morris Waxler is accumulating victim data to start a class action suit against the Refractory Eye Industry and the FDA. Morris Waxler was on the FDA when Lasik was approved by the FDA and has been a champion to stop this Industry.
Would you consider filling out a questionnaire of your complications to be part of the thousands presented in the class action suit against the Industry and FDA. The goal is to stop this Industry.
Please consider contacting morriswaxler@gmail.com and take the survey to document the complications of your eye surgery. He needs YOUR VOICE
I am a physician and am horrified at what I have learned about these barbaric surgeries and ruined lives.
My son, Max Cronin, committed suicide from complications of Lasik/PRK.
I am committed to making a difference in every one’s lives that have been so shattered from this Industry.
I can never get my child back, but maybe I can keep someone else from burying their child or experiencing these devastations.
There are 11 suicides alone in the USA from this…thousands and thousands of victims.
This Industry is backed by Billions of dollars. I am trying to contact victims, so we can bring about unification against this Industry.
nancy, i am so sorry for the loss of your son. words can not express enough …..you say he had the lasik/ prk treatment? i thought the prk was the safest of the options? i ask as i am considering the prk surgery myself..(actually scheduled for friday)..i don’t mean to sound selfish in asking when you have lost so much; but i would love to know if it was actually the prk, or just lasik? thank you for sharing your story , so you can help others.. and again….i am so sorry for your devestating loss. blessings, jennie
Great article; every one makes Lasik seem like a very safe procedure. After reading your article I would say not having any laser surgery is the safest. I would stick to glasses rather than risk vision loss.
Great article. Could I put your article with a link/your graphic… to click on my site and go to your site article? I have 109 marketing websites and 64 million opt-in legal emails. Get you more noticed.
Hey, thanks so much for all this information! I’ve been slowly considering getting vision correction surgery the past couple months, after using contacts for more than 15 years. I’ve always been fine with contacts, mainly because they weren’t expensive for me and because I actually never felt them whenever I wore them (it was as if I wasn’t even wearing them). Given that I was perfectly content with my contacts, the thought of something messing with my eye was kinda disturbing.
But this year I’ve definitely noticed increased moments of having to rub my eyes. They aren’t irritated, but I’m more conscious of them because I’m feeling them more frequently, if that makes sense.
But I’m an engineer both in nature and professionally, so it’s no surprise that I felt the need to get as much information as possible before making a decision, despite people telling me how awesome Lasik was for them. And it bothered me how many people went into a surgery for such a critical part of their body without at LEAST looking into the alternatives. It’s scary to me that someone would choose to buy a Groupon for Lasik surgery because it was on sale, regardless of the number of successful stories and the supposed success rates.
And like you, I also wondered about the minute details. How does the machine know what corrections to make? Every eye is different and will be shaped different, how would the machine know exactly which areas to correct and how much to correct, and what was the resolution of the machine that would map my eye in the first place? How are they cutting the eye? Is it by hand, is it by a machine? How accurate is the machine, how many different types of machines are there? And etc etc.
Just based on initial information, I started leaning toward PRK, and I came upon your site. It’s probably the most thorough explanation I’ve ever seen, and I’m definitely going to use this as a launching point to keep researching some more. So thanks again!!
*thumbs up*, Lois.
We nerds sometimes feel most comfortable knowing the truths that scare the bejeesus out of others.
Keep us posted on your journey!
One thing you don’t really talk about in this article is the claim that PRK exposes you to a greater risk for infection since you’ve taken off the top layer of the eye completely. I’m wondering if that’s really an issue (what is the rate of people who’ve had infections after PRK?).
Or if it is true, is the rate/risk of complications from infections with PRK on par with that from the flap? Yeah, the epilethial layer “heals” quicker with LASIK that prevents longer exposure to possible infections, but you have that corneal flap that never fully heals.
Did you go through with PRK?
I also loved this site and almost got my surgery done. I canceled it the day before. I joined the Facebook group LASIK Complications and learned from the people who actually had the surgery and are now suffering.
I decided to keep my glasses and my contacts. My eyes will be forever healthy. If I were you I would join that group and read EVERYTHING. It will change your mind.
Good luck.
One of the arguments against the no-lasik proponents is the claim that these people had not gotten their procedures done at the best facilities, and that’s why they have had such horrible experiences. What’s your take on it from your time being on that FB group?
And LASIK complications usually only talk about LASIK. I don’t know what the success/complications rate is for PRK as opposed to LASIK.
My take is the following: yes, some of those people went to bad places and some of them went to the best of the best. I had 2 members of my family who had it done in Brazil: one did LASIK and the other did PRK. Both successful.
My decision was based on 2 things: I could not live with any of the complications: halos, dry eye, etc I rather take my contacts off and be free of pain.
The other thing is I am 46 now and will need reading glasses. Plus, if you ever need cataracts surgery, it will make it hard for the doctor to find the perfect lenses. Bottom line is keep your cornea healthy. No laser period.
That Facebook group will show people having all kinds of issues. Do your research.
Mr. Temple,
Thanks a lot for writing such a great article about the various options to correct vision.
I am a post-RK patient that started with a PRK surgery on my left eye first and plan to have it done on the right eye later. For those who might be looking for information on similar experience, you could go to my blog to learn about it:
http://prkafterrk.blogspot.com/
John
Mr. Temple,
Thanks for the your post,Appreciate your work.
What is the maximum myopia power can be corrected with PRK or Trans-PRK.
Doctor who has performed more than 50000 surgeries of all kinds(PRK,LASIK etc.) advised me not to go for PRK as correcting power more than -5 causes haze complication. Does correction of high power causes haze complication? My power is -6.25 -0.5 cyl and -6.5.
Screening results of my cornea thickness at two reputed hospitals are
1)498 left and 506 right
2)523 left and 520 right
Really confused with change in numbers.
Mr. Temple,
How does the Schwind Amaris 1050hz laser compare to the VISX STAR S4 IR laser? One clinic in Vancouver says that the Amaris 1050 is “currently the fastest laser on the market.” While the London Eye Centre states that the VISX STAR S4 IR laser system “represents the most advanced laser technology platform available today.”
Also, if you were to get PRK done today would you still chose the London Eye Centre or another like the Pacific Laser Eye Centre?
I’m not really up to speed on the current versions of the laser systems. Though, the same questions do apply: true correction zone, eye tracking methods, fully-custom treatment map vs preset, etc.
During my research before I had it done, there were two clinics in Vancouver, both using different systems, but both the latest of each, that both seemed a good choice. Ultimately, I went with the ones that did after-care in-house.
If I had to go again, I’d do that same decision process, heavily favouring the after-care in-house. They made tweaks to my steroidal drop regime during my early recovery, based on how my vision was progressing. They do the after-care (short and long-term) for tens of thousands of patients. That’s a lot of expertise. I’m not confident my ophthalmologist, who may have only done a few dozen, would have been able to tailor my recovery. Maybe yes, but definitely has a fraction of the experience.
Honestly the surgery itself is fairly simple (the machines, if they’re up to snuff, do most of the work). I wouldn’t consider going under the photo-knife if I didn’t think the machines and users were going to do it safely, so beyond that, my best possible vision was what I was most concerned about. And it’s the after-care that plays such a huge role in that (again, assuming the surgery has acceptable true correction zone, eye tracking methods, fully-custom treatment map vs preset, etc.)
Thanks. Unfortunately I don’t live in BC and would have to get post-op treatment in another province.
FYI: I found my eyes INCREDIBLY light-sensitive immediately after surgery. I thought I was prepared, but I wasn’t. In the car on the way home, I had on my sports wrap-around sunglasses and over those I had the over-glasses dark glasses too. Even with my eyes shut tightly, my hat pulled low over my eyes, and my head ducked away from the light, I STILL found the bright sunny day painful. Had to get my wife to tinfoil the windows immediately after we got home. This lasted several days.
I say this as a way of underscoring that I would DEFINITELY NOT want to travel those first three days. And days 4 and 5 were quite uncomfortable until the bandage contact lens was taken off (though I could handle the light).
YMMV, but consider very, very strongly staying in town for at least three days post-op (ideally five). Knowing what I know now, I would postpone the surgery until I could stay in town.
Much appreciated!!!
Hi. Thanks for the great article. So just to clarify: does the eye completely heal with epi-LASIK and LASEK the way it does with PRK? It’s just LASIK that leaves permanent damage/flap?
After doing extensive research I decided not to have ANY sort of lasik surgery. I learned a lot from this group:
https://www.facebook.com/groups/LasikComplicationsFaceBookGroup/
LASIK/PRK or whatever… will damage your eyes for good. Keep your eyes healthy.
Good luck.
Hello Mr. Temple,
Great article, I only recently was planning to get LASIK done and after reading your article decided to chose PRK. I think it was a good choice, I am now one week into the PRK and while it will take a while to get to 20/20 vision I am happy that your article brought forward the clear and concise facts, letting the patient make the final decision.
I like yourself like to dig deep into information before I make my mind up, and being a prfessional in the engineering field I feel your article provide the due diligence needed to carry out LASIK/PRK or other surgery.
Keep up the good work
Ums
There are no nerves severed by these procedures. The nervous layer of the eye resides entirely within the interior cavity and does not extend through the lens or cornea. This information is incorrect and creates suspicion as to the credibility of sources and the validity of statements and quotes presented as factual in this article.
Ten seconds of googling reveals the following study (by Lasik doctors).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3911824/
They’re not debating WHETHER nerves are damage/altered/cut, they all know it happens. They’re comparing the amount of decrease in nerve density after the flap creation by various methods.
And they conclude that ALL methods of flap creation affect the nerve density:
“Nerve density was decreased at 1 month compared to preoperative and remained decreased through 12 months”
If you have a reputable source that suggests nerves are unaffected by the flap-cut, I would be interested in reading it.
if you hadn’t had your surgery, would you still have it today?
Absolutely. But I’d never have a surgery that involves a cornea flap.
Seriously fab and intelligent article. This kind of consumer-takes-industry-by-the-horns-with-derring-do writing is precisely why I still believe in the internet. Thank you so much, and I will be sure to share the dangers of LASIK with everyone I know, & I feel extremely excited to further research PRK.
Cheers!
Mr. Temple,
As a US Military servicemember, any eye treatment is free for me. I underwent LASIK in 1999. I’ve had no issues, and absolutely loved it…I just wish I had this article then…My question to you is, I would like to get an enhancement, and that’s how I stumbled upon this article. Travelling overseas to do it, plus the cost of the procedure is not really an option for me. Would you recommend PRK or just going to glasses or contacts? Just curious. Thanks.
I don’t really know anything about touchups after Lasik. I know they’re effectively no different for PRK (skin is removed, then cornea surface is touched-up).
I’d do a lot of reading into the potential complications. If you’ve had no flap issues or epithelial ingrowth or issues with the remaining thickness of cornea, that may not be the same if they lift the flap to do another Lasik.
At minimum with Lasik, they’re going to be treating your remaining cornea, which is already quite thinner after the first lasik. The amount removed for the correction is the same with PRK or with Lasik, but obviously if you take that same amount off from the middle of the cornea, it’s going to be a much higher percentage of the remaining cornea than if you took it off the outside of the cornea.
Definitely do some checking into PRK over Lasik. I don’t know if that’s even possible, but my common-sense understanding of the procedures suggests it could be less risky than opening up the flap to do Lasik a second time. Who knows though, whether PRK on a flap is still safe enough to warrant the surgery.
Back in 1999 , they mostly did PRK anyways, the flap technique is relatively new .
Over all what would you recommend age wise to be before getting corrective surgery?
Mr. Temple,
Thank you for doing your homework and writing this. I recently had an evaluation to determine if I was a candidate for Lasik/PRK. I have several friends and family that have undergone Lasik in the last 2 years and once I finally saved up the money, I was gung-ho with having the Lasik procedure done myself. In fact, I was very anti-PRK because, well… just because! I had heard so many good things about Lasik and those I talked to simply said that PRK is really a back-up if you are not a candidate for Lasik, but that it takes longer to heal, and why would one want that?
At my evaluation, the doctor that I saw told me that I was a candidate for either, but he would recommend PRK because there was no reason NOT to do PRK over Lasik. I was thrown by this because I had been a firm believer that Lasik was the best way to go and I didn’t expect to be advised down the PRK route unless there was some medical reason for it. When I voiced my concern about this, the doctor informed me about the potential for future issues that stem from Lasik (those you mention in your article) and said that, for the most part, those doctors who push Lasik over PRK are only in it for the money.
After asking more questions about PRK and receiving satisfactory answers, I put my initial shock/fears aside and signed the paperwork. However, once I started relaying to family members who knew I was signing up for the procedure, I started doubting the decision (though, not enough to back out!). This article has helped ease those doubts and has made me feel confident in my upcoming procedure, so THANK YOU!
I disagree that corneal flap never heals because I have Lasik done twice in 6 months. When I have allergies, I rub my eyes very hard. If this article’s claims are true, rubbing eyes that hard would have dislodged the flap. I do agree with thickness issue.
Hi there. I’m glad you have had no issues yet, but you have been misinformed about the procedure done to your eyes.
The skin over your cornea-flap heals very quickly after Lasik, but the cut in the cornea itself will never heal.
There are numerous studies done and much work and study performed by Lasik doctors to reduce the permanent effects and potential side-effects of this never-healing cornea flap.
My advice to you is to not assume your eyes are structurally the same as they were before.
They are not.
See the citations in these articles from Lasik journals describing relatively minor rubbing or impacts to post-lasik eyes, which have dislodged the cornea flap, sometimes many, many years post surgery.
Do some more study and ask some impartial doctors about what you can do to mitigate the risks.
This is interesting. I had my LASIK done at Lasik Plus in Westbury, Long Island NY in 2007
I was very satisfied, perhaps dryer eyes and I once had a stye after. But by and large I was pleased very much and had no noticeable issues. I am now 33 and my eyes upon a DMV required test showed I needed some aid. In contacts I need -.75 and-.50 so it not a lot and I forgot my original time of surgery need. Maybe a full point and .50 negative.
They offer PRK for me to retouch, but I am scared and now looking at other information since the internet has BOOMED since 2007 even more and possibly the surgeries and technology for the procedure and studies. I’m still unclear what to do especially since I am older and my activity levels are forced to decline because of joint diseases– I danced a lot in my life– not uncommon– that I won’t need as frequent unencumbered vision aid. It is hard reality. But this is life. I’ll keep my eyes open ….
I had LASIK 20 years ago, with no problems. Had blepheroplasty 2017, have had severe dry eyes ever since. Have been told by an experienced eye specialist, my current symptoms are related to the LASIK done 20 years ago.
So please do not do LASIK or blepheroplasy, keep yours eyes healthy, wear glasses, and age gracefully!
Thank you very much for all the research and the effort to share the information to other people.
It really helps a lot and I highly appreciate it!!